14 June is World Blood Donor Day.
Stable supplies of safe blood allow healthcare systems to be better equipped to handle obstetric health crises, including severe bleeding after childbirth, and provide quality care to women.
Many women who bleed severely after childbirth rely on blood donations to replace the blood they have lost.
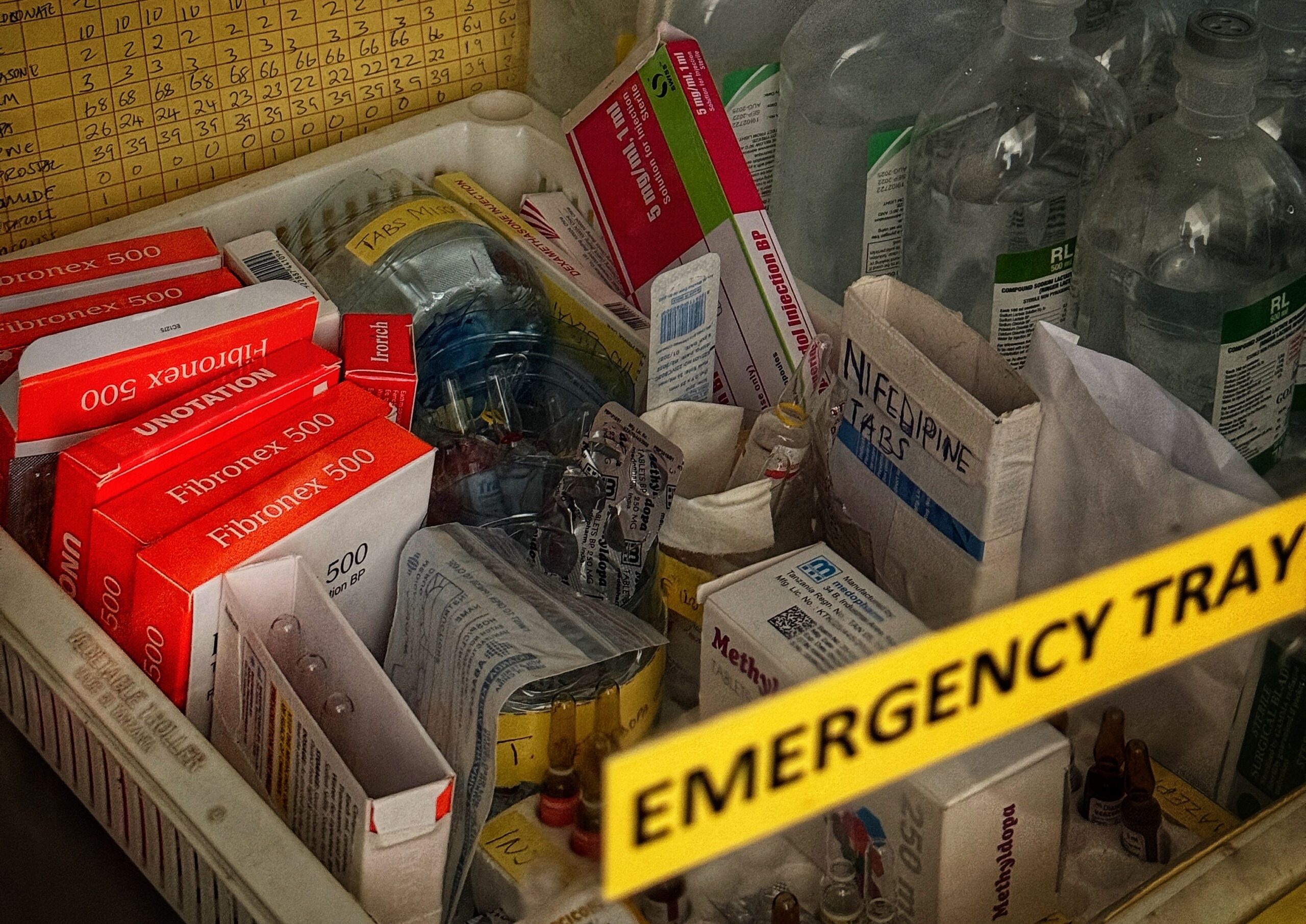
However, to alleviate the pressure on blood stocks, which are not always available, tranexamic acid (TXA), a drug used to reduce life-threatening bleeding, can be used.
TXA can be used earlier before a blood transfusion is needed. It also has the potential to reduce costs incurred from procuring blood, particularly in countries where blood transfusions are scarce for mothers who experience severe blood loss after birth and must pay out-of-pocket to receive a blood transfusion.
Experts based at the Clinical Trials Unit (CTU) at the London School of Hygiene & Tropical Medicine (LSHTM) and the WOMAN Trial’s National Coordinating Centre in Nigeria explain more.
1. TXA could alleviate pressure on blood stocks
When there is no blood available, TXA can be used much earlier to reduce bleeding and prevent the need for a blood transfusion.
The World Health Organization guidelines on postpartum haemorrhage (PPH) states that TXA should be the first option to reduce severe blood loss
This is also an issue in other areas of healthcare where surgery occurs. At least one third of surgical patients in the UK who should receive TXA are not treated, with half a million surgical patients in the UK missing out on its benefits, according to an article published in the British Medical Journal last year.
Professor Ian Roberts, Co-Lead of the WOMAN Trials, said:
“Surveys have shown that many patients want to avoid blood transfusions and, in some circumstances in the UK, surgeries are cancelled because of low blood stocks.
“The failure to use TXA more widely in these instances is a failure of patient care.”
An earlier 2012 systematic review produced strong evidence showing that TXA reduces the risk of blood transfusion needed in surgery by up to one third, thus also reducing the duration of anaesthesia, the need for intensive care and increasing early discharge from hospital facilities.
Professor Roberts gave evidence at the UK’s Infected Blood Inquiry in 2024 to improve patient safety by recommending blood transfusion practitioners in England include TXA in hospital surgical checklists.
This is informed by evidence that TXA reduces major surgical bleeding by one quarter.
Blood transfusions are vital for millions of people undergoing surgery, but there is currently a national shortage in the UK.
The NHS called for 200,000 more blood donors after it issued an ‘amber alert’ on blood shortages on Monday, with regular donors needing to increase from around 800,000 to over one million to maintain stable blood supplies.
2. TXA could reduce costs on paying for blood out-of-pocket

More access to TXA could help hospitals cut costs in procuring blood and save families from needing to donate blood for their relatives.
Professor Nike Bello, a gynaecologist and obstetrician based at University College Hospital, Ibadan and Co-lead of the WOMAN Trials in Nigeria said: “If you fall into labour in the middle of the night, you just have no one to get you to hospital.
“And then when you get to the hospital itself, [there is no] ability to afford the blood transfusion, what you need for emergency surgery, for safe delivery.

In Nigeria, healthcare is not affordable and accessible to many citizens despite there being a National Health Insurance Scheme, “but not everyone subscribes”, says Professor Bello.
She concludes: “If you cannot pay out-of-pocket, you don’t get the healthcare you need.”
Further, women are expected to have at least two pints of blood in reserve before they are accepted by the hospital.
This leaves many women and families to pay for blood or rely on a relative to donate their own.
3. TXA can quickly reduce severe bleeding if given early

In 2017, the WOMAN Trial found TXA reduces death from bleeding and the need for surgery to control bleeding by about one third when given to women with PPH within three hours of birth.
TXA reduces bleeding by inhibiting the breakdown of blood clots.
Using TXA instead of a blood transfusion can also reduce the risk of giving a patient contaminated blood and simplify the process of finding the right blood group for a patient.

Dr Asfifa Dayan Khan, Assistant Professor in Surgery at Holy Family Hospital, who is part of the WOMAN Trial team in Pakistan said: “Many times, we think that it’s [a transfusion] just a simple case, [but] we don’t get the blood group.
“We have to rush to the blood bank, not only to get the blood group, but to arrange the blood and get the crossmatch done.”
Find out more about how the CTU’s global clinical trials are assessing how TXA can save more lives from severe bleeding.